

- RFQ
- BOM
-
Contact Us
Tel: +86-0755-83501315
Email: sales@sic-components.com
- Chinese
- English
- French
- German
- Portuguese
- Spanish
- Russian
- Japanese
- Korean
- Arabic
- Irish
- Greek
- Turkish
- Italian
- Danish
- Romanian
- Indonesian
- Czech
- Afrikaans
- Swedish
- Polish
- Basque
- Catalan
- Esperanto
- Hindi
- Lao
- Albanian
- Amharic
- Armenian
- Azerbaijani
- Belarusian
- Bengali
- Bosnian
- Bulgarian
- Cebuano
- Chichewa
- Corsican
- Croatian
- Dutch
- Estonian
- Filipino
- Finnish
- Frisian
- Galician
- Georgian
- Gujarati
- Haitian
- Hausa
- Hawaiian
- Hebrew
- Hmong
- Hungarian
- Icelandic
- Igbo
- Javanese
- Kannada
- Kazakh
- Khmer
- Kurdish
- Kyrgyz
- Latin
- Latvian
- Lithuanian
- Luxembou..
- Macedonian
- Malagasy
- Malay
- Malayalam
- Maltese
- Maori
- Marathi
- Mongolian
- Burmese
- Nepali
- Norwegian
- Pashto
- Persian
- Punjabi
- Serbian
- Sesotho
- Sinhala
- Slovak
- Slovenian
- Somali
- Samoan
- Scots Gaelic
- Shona
- Sindhi
- Sundanese
- Swahili
- Tajik
- Tamil
- Telugu
- Thai
- Ukrainian
- Urdu
- Uzbek
- Vietnamese
- Welsh
- Xhosa
- Yiddish
- Yoruba
- Zulu
- Kinyarwanda
- Tatar
- Oriya
- Turkmen
- Uyghur
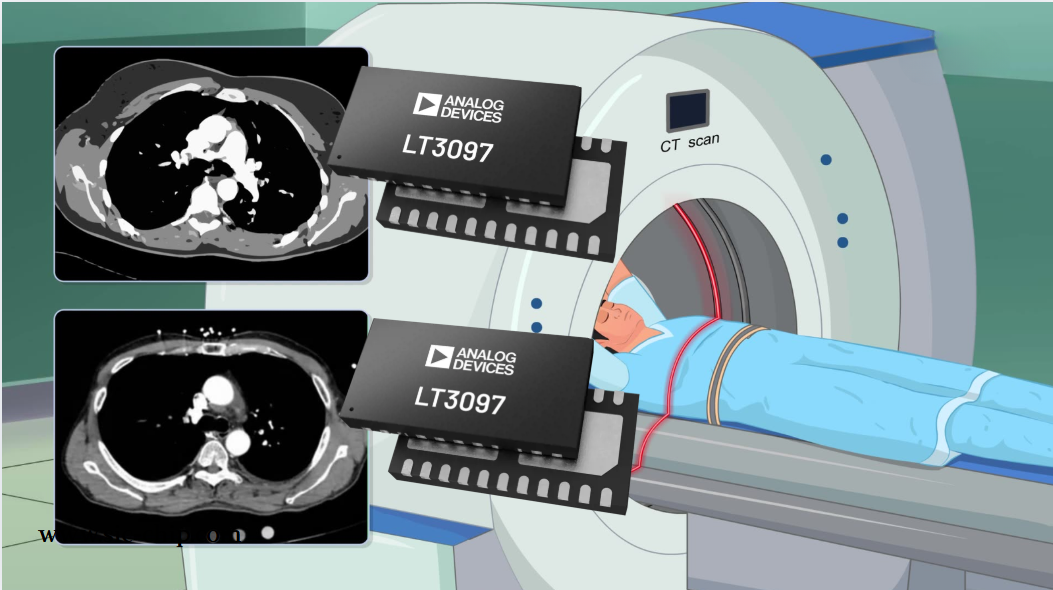
How to Improve Medical Imaging With Precision Amplifiers?
In the field of medical imaging, the role of precision amplifiers goes far beyond simply making images sharper—they are the core that captures those faint yet critical signals, the ones that may hold clues to early diagnosis but are easily drowned out by noise or overshadowed by irrelevant data. The essence of medical imaging is to convert physical phenomena, such as X-ray photons, MRI signals, or ultrasound echoes, into electrical signals that can be processed into images. And precision amplifiers are the bridge that transforms these weak signals into something meaningful.
Signals in medical imaging are often extremely faint. Think about MRI equipment—the radiofrequency signals emitted by hydrogen atoms in the human body are measured in microvolts or even nanovolts. Ordinary amplifiers would simply drown these signals in their own noise, making potential tumor markers indistinct. But precision amplifiers are different; they are designed with ultra-low noise floors, possibly as low as 1nV/√Hz or even lower. This means they can amplify weak signals without introducing so much noise of their own that the signal becomes muddled. I’ve seen many MRI images where, after switching to a low-noise amplifier, a previously blurry shadow transformed into a clear lesion—this isn’t some kind of magic, just giving the signal a chance to be seen.
Linearity is also crucial. The accuracy of medical images is too important—a tiny change in brightness can represent a significant difference in tissue density. If an amplifier distorts the signal, making small inputs appear larger than they actually are or vice versa, the image becomes untrustworthy. Precision amplifiers, with their high linearity, can maintain the true relationship between input and output, not favoring any signal strength, just amplifying evenly. This is particularly evident in X-ray imaging, where subtle differences in photon absorption can distinguish between healthy bone and a fracture. A non-linear amplifier might make a hairline crack disappear or exaggerate a harmless density anomaly—either scenario could lead to misdiagnosis.
Dynamic range is another point that cannot be ignored. Medical imaging systems often have to handle signal intensities over an extremely wide range. In ultrasound, for example, the echoes from shallow tissues are strong, while those from deeper structures are much weaker. An amplifier with a narrow dynamic range would either clip the strong signals or let the weak ones vanish into noise. The high dynamic range of precision amplifiers, however, can handle both extremes, amplifying weak echoes enough to be visible without distorting the strong ones. It’s like a camera that can capture details in both bright sunlight and dark corners, but focused on the inside of the human body.
Offset voltage and drift are easy to overlook, but they have a huge impact on long-term stability. Imagine a system that requires long-term monitoring, such as observing tumor growth through regular scans. If the amplifier’s offset voltage drifts with temperature or usage time, the baseline signal will change, making it difficult to compare images. Precision amplifiers use techniques like laser trimming or temperature-compensated components to reduce such drift; the initial offset voltage may be only a few microvolts, and it can remain stable even after the device has been running for hours. In some systems I’ve worked with, this stability determined whether a 1-millimeter growth could be detected or completely missed.
Common-mode rejection ratio is nothing short of an unsung hero in noisy clinical environments. Hospitals are full of electronic interference—monitoring devices, infusion pumps, even the MRI magnet itself can generate common-mode signals that mix into the sensor output. A precision amplifier with a high common-mode rejection ratio (CMRR) can filter out this noise, focusing only on the differential signal from the sensor. This is especially important in EEG or ECG imaging, where signals are inherently weak and prone to interference. A high CMRR amplifier can turn a jagged, noisy trace into a clean waveform that doctors can interpret with confidence.
Compatibility with other components is also critical. Modern medical imaging systems are complex, with sensors, analog-to-digital converters (ADCs), and processing units all needing to work together. Those precision amplifiers that easily interface with ADCs, possibly with built-in gain settings or low output impedance, can simplify the design and avoid introducing additional noise or delay when the signal is passed to the next stage. No matter how good the amplifier itself is, a poor match with the ADC can turn a clean signal into a jumbled mess.
Choosing the right amplifier depends on the needs of the specific imaging method, much like selecting key parts for a precision instrument. ADI’s AD8253 is a good choice, with a noise level of 3nV/√Hz, a CMRR as high as 130dB, and a wide power supply range from ±2.25V to ±18V, making it particularly suitable for ECG/EEG signal acquisition and portable medical devices. It has an ultra-low offset voltage of only 50μV and comes with temperature compensation, allowing it to maintain a stable baseline even during long-term monitoring. I once used it in a wearable ECG device, and the waveform recorded continuously for 24 hours showed almost no drift, providing solid data for the diagnosis of arrhythmias.
TI’s OPA2388 is also excellent, with noise as low as 0.9nV/√Hz, an open-loop gain of 130dB, and rail-to-rail output. It’s a real workhorse when dealing with nanovolt-level MRI signals. In one project, traditional amplifiers resulted in images with low signal-to-noise ratios and blurry tumor boundaries; after switching to the OPA2388, the noise level decreased by 60%, and small lesions became clearly visible—it was like putting a pair of high-definition glasses on the MRI, making it particularly suitable for pre-amplification in MRI receiver coils and high-sensitivity ultrasound probes.
For TGC circuits in ultrasound imaging systems or multi-channel physiological signal acquisition, ADI’s AD8253 is a good fit. It’s a 4-channel programmable gain amplifier with a gain range of 0.5 to 128 and a power consumption of only 5mA per channel. The multi-channel integrated design can greatly simplify the ultrasound front-end circuit, and the gain of each channel can be independently programmed, which is perfect for compensating for echo attenuation in tissues at different depths. I used it in a 32-channel ultrasound system, which saved 30% of PCB space compared to a discrete solution, and the consistency between channels was much better.
TI’s THS4521 is a high-speed transimpedance amplifier with a noise level of 1.1nV/√Hz and a slew rate of up to 1700V/μs, designed specifically for high-frequency optical signal detection. Its 1.2GHz bandwidth can capture nanosecond-level optical pulses. It performs well in photodiode signal processing in CT scanners or fluorescence detection equipment. A portable fluorescence immunoassay analyzer using it reduced the detection time from 5 minutes to 30 seconds while maintaining picoampere-level current detection sensitivity.
For implantable medical devices or remote health monitoring patches, TI’s INA333 is more suitable. It’s a micro-power instrumentation amplifier with a current of only 17μA, capable of rail-to-rail input and output, and with built-in gain-setting resistors. Its ultra-low power consumption makes it an ideal choice for battery-powered devices. A wearable blood glucose monitoring patch using it can work continuously for 14 days on a single CR2032 battery, and the built-in gain resistors eliminate the need for external components, saving a lot of space on the millimeter-sized PCB.
When choosing, for noise-sensitive applications such as MRI or EEG, AD8253 or OPA2388 are more reliable, with a noise density below 1nV/√Hz being the key indicator. For multi-channel applications like ultrasound or multi-lead ECG, the 4-channel PGA design of AD8253 can save a lot of trouble. For portable or implantable devices, the low power consumption of INA333 is unparalleled; when paired with low-voltage power supply, it can significantly extend battery life. For high-speed signal processing such as CT or laser imaging, the GHz-level bandwidth and high slew rate of THS4521 are essential.
However, just looking at parameter tables isn’t enough; it’s best to actually build a circuit for testing. In ECG applications, for example, two amplifiers with similar noise indicators but different CMRRs can have vastly different abilities to resist myoelectric interference. Moreover, medical devices have a long lifecycle, often 5 to 10 years, so supply chain stability must also be considered to avoid product iteration risks due to chip discontinuation. When developing a portable ultrasound diagnostic instrument, SIC’s partner manufacturers hesitated between AD8253 and its competitors; tests showed that the inter-channel gain matching error of AD8253 was less than 0.1%, much better than the competitor’s 0.5%, significantly improving the uniformity of deep tissue imaging. There’s also a long-term implantable EEG monitoring system that uses INA333, extending the battery replacement cycle from once a month to once every six months, greatly reducing the burden on patients.
In the end, the right precision amplifiers are the unsung heroes of medical imaging systems, quietly improving image quality and giving doctors more confidence in making accurate diagnoses. Every time a doctor detects a problem early because the image is clear and accurate, there are these amplifiers working silently behind the scenes, unassuming yet vital.
AD8253: https://www.sic-components.com/product/search?search=AD8253ARMZ
INA333: https://www.sic-components.com/product/product?product_id=1888776
OPA2388: https://www.sic-components.com/product/product?product_id=13237260
THS452: https://www.sic-components.com/product/product?product_id=1991525
Hot Products
View MoreRelated Blogs

2000+
Daily average RFQ Volume

30,000,000
Standard Product Unit

2800+
Worldwide Manufacturers

15,000 m2
In-stock Warehouse






 Wishlist (0 Items)
Wishlist (0 Items) 